Subtitles & vocabulary
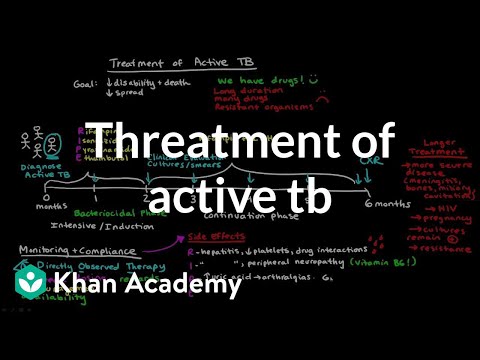
Treatment of Active TB | Infectious diseases | NCLEX-RN | Khan Academy
00
廖芯琳 posted on 2017/03/15Save
Video vocabulary
sort
US /sɔrt/
・
UK /sɔ:t/
- Transitive Verb
- To organize things by putting them into groups
- To deal with things in an organized way
- Noun
- Group or class of similar things or people
A1TOEIC
More chronic
US /ˈkrɑnɪk/
・
UK /'krɒnɪk/
- Adjective
- Always or often doing something, e.g. lying
- (Of disease) over a long time; serious
B1
More recognize
US /ˈrek.əɡ.naɪz/
・
UK /ˈrek.əɡ.naɪz/
- Transitive Verb
- To accept the truth or reality of something
- To consider something as important or special
A2TOEIC
More period
US /ˈpɪriəd/
・
UK /ˈpɪəriəd/
- Noun (Countable/Uncountable)
- Set amount of time during which events take place
- A way to emphasize what you will say
A1TOEIC
More Use Energy
Unlock Vocabulary
Unlock pronunciation, explanations, and filters
